Alcoholism
| Alcoholism | |
|---|---|
| Other names | Alcohol addiction, alcohol dependence syndrome, alcohol use disorder (AUD)[1] |
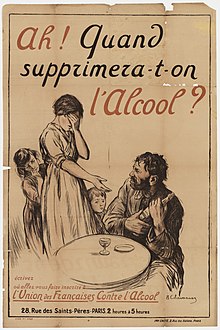 | |
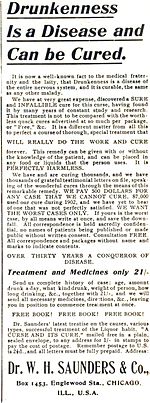
| A French temperance organisation poster depicting the effects of alcoholism in a family, c. 1915: "Ah! When will we be rid of alcohol?" | |
| Specialty | Psychiatry, clinical psychology, toxicology, addiction medicine |
| Symptoms | Drinking large amounts of alcohol over a long period, difficulty cutting down, acquiring and drinking alcohol taking up a lot of time, usage resulting in problems, withdrawal occurring when stopping[2] |
| Complications | Mental illness, delirium, Wernicke–Korsakoff syndrome, irregular heartbeat, cirrhosis of the liver, cancer, fetal alcohol spectrum disorder, suicide[3][4][5][6] |
| Duration | Long term[2] |
| Causes | Environmental and genetic factors[4] |
| Risk factors | Stress, anxiety, easy access[4][7] |
| Diagnostic method | Questionnaires, blood tests[4] |
| Treatment | Alcohol cessation typically with benzodiazepines, counselling, acamprosate, disulfiram, naltrexone[8][9][10] Alcoholics Anonymous (AA) and other Twelve Step Programs, AA/Twelve Step Facilitation (AA/TSF)[11] |
| Frequency | 380 million / 5.1% adults (2016)[12][13] |
| Deaths | 3.3 million / 5.9%[14] |
Alcoholism is the continued drinking of alcohol despite it causing problems. Some definitions require evidence of dependence and withdrawal.[15] Problematic use of alcohol has been mentioned in the earliest historical records. The World Health Organization (WHO) estimated there were 283 million people with alcohol use disorders worldwide as of 2016[update].[12][13] The term alcoholism was first coined in 1852,[16] but alcoholism and alcoholic are sometimes considered stigmatizing and to discourage seeking treatment, so diagnostic terms such as alcohol use disorder or alcohol dependence are often used instead in a clinical context.[17][18][19]
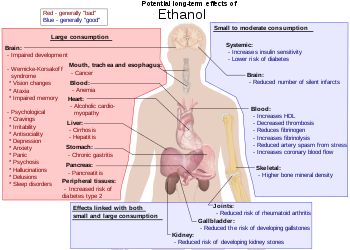
Alcohol is addictive, and heavy long-term alcohol use results in many negative health and social consequences. It can damage all the organ systems, but especially affects the brain, heart, liver, pancreas and immune system.[4][5] Heavy alcohol usage can result in trouble sleeping, and severe cognitive issues like dementia, brain damage, or Wernicke–Korsakoff syndrome. Physical effects include irregular heartbeat, an impaired immune response, liver cirrhosis, increased cancer risk, and severe withdrawal symptoms if stopped suddenly.[4][5][20] These health effects can reduce life expectancy by 10 years.[21] Drinking during pregnancy may harm the child's health,[3] and drunk driving increases the risk of traffic accidents. Alcoholism is also associated with increases in violent and non-violent crime.[22] While alcoholism directly resulted in 139,000 deaths worldwide in 2013,[23] in 2012 3.3 million deaths may be attributable globally to alcohol.[14]
The development of alcoholism is attributed to both environment and genetics equally.[4] The use of alcohol to self-medicate stress or anxiety can turn into alcoholism.[24] Someone with a parent or sibling with an alcohol use disorder is three to four times more likely to develop an alcohol use disorder themselves, but only a minority of them do.[4] Environmental factors include social, cultural and behavioral influences.[25] High stress levels and anxiety, as well as alcohol's inexpensive cost and easy accessibility, increase the risk.[4][7] People may continue to drink partly to prevent or improve symptoms of withdrawal.[4] After a person stops drinking alcohol, they may experience a low level of withdrawal lasting for months.[4] Medically, alcoholism is considered both a physical and mental illness.[26][27] Questionnaires are usually used to detect possible alcoholism.[4][28] Further information is then collected to confirm the diagnosis.[4]
Treatment of alcoholism may take several forms.[9] Due to medical problems that can occur during withdrawal, alcohol cessation should be controlled carefully.[9] One common method involves the use of benzodiazepine medications, such as diazepam.[9] These can be taken while admitted to a health care institution or individually.[9] The medications acamprosate or disulfiram may also be used to help prevent further drinking.[10] Mental illness or other addictions may complicate treatment.[29] Various individual or group therapy or support groups are used to attempt to keep a person from returning to alcoholism.[8][30] Among them is the abstinence based mutual aid fellowship Alcoholics Anonymous (AA). A 2020 scientific review found that clinical interventions encouraging increased participation in AA (AA/twelve step facilitation (AA/TSF))—resulted in higher abstinence rates over other clinical interventions, and most studies in the review found that AA/TSF led to lower health costs.[a][32][33][34]
Many terms, some slurs and some informal, have been used to refer to people affected by alcoholism such as tippler, drunkard, dipsomaniac and souse.[35]
Signs and symptoms
The risk of alcohol dependence begins at low levels of drinking and increases directly with both the volume of alcohol consumed and a pattern of drinking larger amounts on an occasion, to the point of intoxication, which is sometimes called binge drinking. Binge drinking is the most common pattern of alcoholism. It has different definitions and one of this defines it as a pattern of drinking when a male has five or more drinks on an occasion or a female has at least four drinks on an occasion.[36]
Long-term misuse
Alcoholism is characterized by an increased tolerance to alcohol – which means that an individual can consume more alcohol – and physical dependence on alcohol, which makes it hard for an individual to control their consumption. The physical dependency caused by alcohol can lead to an affected individual having a very strong urge to drink alcohol. These characteristics play a role in decreasing the ability to stop drinking of an individual with an alcohol use disorder.[37] Alcoholism can have adverse effects on mental health, contributing to psychiatric disorders and increasing the risk of suicide. A depressed mood is a common symptom of heavy alcohol drinkers.[38][39]
Warning signs
Warning signs of alcoholism include the consumption of increasing amounts of alcohol and frequent intoxication, preoccupation with drinking to the exclusion of other activities, promises to quit drinking and failure to keep those promises, the inability to remember what was said or done while drinking (colloquially known as "blackouts"), personality changes associated with drinking, denial or the making of excuses for drinking, the refusal to admit excessive drinking, dysfunction or other problems at work or school, the loss of interest in personal appearance or hygiene, marital and economic problems, and the complaint of poor health, with loss of appetite, respiratory infections, or increased anxiety.[40]
Physical
Short-term effects
Drinking enough to cause a blood alcohol concentration (BAC) of 0.03–0.12% typically causes an overall improvement in mood and possible euphoria (intense feelings of well-being and happiness), increased self-confidence and sociability, decreased anxiety, a flushed, red appearance in the face and impaired judgment and fine muscle coordination. A BAC of 0.09% to 0.25% causes lethargy, sedation, balance problems and blurred vision. A BAC of 0.18% to 0.30% causes profound confusion, impaired speech (e.g. slurred speech), staggering, dizziness and vomiting. A BAC from 0.25% to 0.40% causes stupor, unconsciousness, anterograde amnesia, vomiting (death may occur due to inhalation of vomit while unconscious) and respiratory depression (potentially life-threatening). A BAC from 0.35% to 0.80% causes a coma (unconsciousness), life-threatening respiratory depression and possibly fatal alcohol poisoning. With all alcoholic beverages, drinking while driving, operating an aircraft or heavy machinery increases the risk of an accident; many countries have penalties for drunk driving.
Long-term effects
Having more than one drink a day for women or two drinks for men increases the risk of heart disease, high blood pressure, atrial fibrillation, and stroke.[41] Risk is greater with binge drinking, which may also result in violence or accidents. About 3.3 million deaths (5.9% of all deaths) are believed to be due to alcohol each year.[14] Alcoholism reduces a person's life expectancy by around ten years[21] and alcohol use is the third leading cause of early death in the United States.[41] Long-term alcohol misuse can cause a number of physical symptoms, including cirrhosis of the liver, pancreatitis, epilepsy, polyneuropathy, alcoholic dementia, heart disease, nutritional deficiencies, peptic ulcers[42] and sexual dysfunction, and can eventually be fatal. Other physical effects include an increased risk of developing cardiovascular disease, malabsorption, alcoholic liver disease, and several cancers such as breast cancer and head and neck cancer.[43] Damage to the central nervous system and peripheral nervous system can occur from sustained alcohol consumption.[44][45] A wide range of immunologic defects can result and there may be a generalized skeletal fragility, in addition to a recognized tendency to accidental injury, resulting in a propensity for bone fractures.[46]
Women develop long-term complications of alcohol dependence more rapidly than do men, women also have a higher mortality rate from alcoholism than men.[47] Examples of long-term complications include brain, heart, and liver damage[48] and an increased risk of breast cancer. Additionally, heavy drinking over time has been found to have a negative effect on reproductive functioning in women. This results in reproductive dysfunction such as anovulation, decreased ovarian mass, problems or irregularity of the menstrual cycle, and early menopause.[47] Alcoholic ketoacidosis can occur in individuals who chronically misuse alcohol and have a recent history of binge drinking.[49][50] The amount of alcohol that can be biologically processed and its effects differ between sexes. Equal dosages of alcohol consumed by men and women generally result in women having higher blood alcohol concentrations (BACs), since women generally have a lower weight and higher percentage of body fat and therefore a lower volume of distribution for alcohol than men.[51]
Psychiatric
Long-term misuse of alcohol can cause a wide range of mental health problems. Severe cognitive problems are common; approximately 10% of all dementia cases are related to alcohol consumption, making it the second leading cause of dementia.[52] Excessive alcohol use causes damage to brain function, and psychological health can be increasingly affected over time.[53] Social skills are significantly impaired in people with alcoholism due to the neurotoxic effects of alcohol on the brain, especially the prefrontal cortex area of the brain. The social skills that are impaired by alcohol use disorder include impairments in perceiving facial emotions, prosody, perception problems, and theory of mind deficits; the ability to understand humor is also impaired in people who misuse alcohol.[54] Psychiatric disorders are common in people with alcohol use disorders, with as many as 25% also having severe psychiatric disturbances. The most prevalent psychiatric symptoms are anxiety and depression disorders. Psychiatric symptoms usually initially worsen during alcohol withdrawal, but typically improve or disappear with continued abstinence.[55] Psychosis, confusion, and organic brain syndrome may be caused by alcohol misuse, which can lead to a misdiagnosis such as schizophrenia.[56] Panic disorder can develop or worsen as a direct result of long-term alcohol misuse.[57][58]
The co-occurrence of major depressive disorder and alcoholism is well documented.[59][60][61] Among those with comorbid occurrences, a distinction is commonly made between depressive episodes that remit with alcohol abstinence ("substance-induced"), and depressive episodes that are primary and do not remit with abstinence ("independent" episodes).[62][63][64] Additional use of other drugs may increase the risk of depression.[65] Psychiatric disorders differ depending on gender. Women who have alcohol-use disorders often have a co-occurring psychiatric diagnosis such as major depression, anxiety, panic disorder, bulimia, post-traumatic stress disorder (PTSD), or borderline personality disorder. Men with alcohol-use disorders more often have a co-occurring diagnosis of narcissistic or antisocial personality disorder, bipolar disorder, schizophrenia, impulse disorders or attention deficit/hyperactivity disorder (ADHD).[66] Women with alcohol use disorder are more likely to experience physical or sexual assault, abuse, and domestic violence than women in the general population,[66] which can lead to higher instances of psychiatric disorders and greater dependence on alcohol.
Social effects
Serious social problems arise from alcohol use disorder; these dilemmas are caused by the pathological changes in the brain and the intoxicating effects of alcohol.[52][67] Alcohol misuse is associated with an increased risk of committing criminal offences, including child abuse, domestic violence, rape, burglary and assault.[68] Alcoholism is associated with loss of employment,[69] which can lead to financial problems. Drinking at inappropriate times and behavior caused by reduced judgment can lead to legal consequences, such as criminal charges for drunk driving[70] or public disorder, or civil penalties for tortious behavior. An alcoholic's behavior and mental impairment while drunk can profoundly affect those surrounding him and lead to isolation from family and friends. This isolation can lead to marital conflict and divorce, or contribute to domestic violence. Alcoholism can also lead to child neglect, with subsequent lasting damage to the emotional development of children of people with alcohol use disorders.[71] For this reason, children of people with alcohol use disorders can develop a number of emotional problems. For example, they can become afraid of their parents, because of their unstable mood behaviors. They may develop shame over their inadequacy to liberate their parents from alcoholism and, as a result of this, may develop self-image problems, which can lead to depression.[72]
Alcohol withdrawal
As with similar substances with a sedative-hypnotic mechanism, such as barbiturates and benzodiazepines, withdrawal from alcohol dependence can be fatal if it is not properly managed.[67][73] Alcohol's primary effect is the increase in stimulation of the GABAA receptor, promoting central nervous system depression. With repeated heavy consumption of alcohol, these receptors are desensitized and reduced in number, resulting in tolerance and physical dependence. When alcohol consumption is stopped too abruptly, the person's nervous system experiences uncontrolled synapse firing. This can result in symptoms that include anxiety, life-threatening seizures, delirium tremens, hallucinations, shakes and possible heart failure.[74][75] Other neurotransmitter systems are also involved, especially dopamine, NMDA and glutamate.[37][76]
Severe acute withdrawal symptoms such as delirium tremens and seizures rarely occur after 1-week post cessation of alcohol. The acute withdrawal phase can be defined as lasting between one and three weeks. In the period of 3–6 weeks following cessation, anxiety, depression, fatigue, and sleep disturbance are common.[77] Similar post-acute withdrawal symptoms have also been observed in animal models of alcohol dependence and withdrawal.[78]
A kindling effect also occurs in people with alcohol use disorders whereby each subsequent withdrawal syndrome is more severe than the previous withdrawal episode; this is due to neuroadaptations which occur as a result of periods of abstinence followed by re-exposure to alcohol. Individuals who have had multiple withdrawal episodes are more likely to develop seizures and experience more severe anxiety during withdrawal from alcohol than alcohol-dependent individuals without a history of past alcohol withdrawal episodes. The kindling effect leads to persistent functional changes in brain neural circuits as well as to gene expression.[79] Kindling also results in the intensification of psychological symptoms of alcohol withdrawal.[77] There are decision tools and questionnaires that help guide physicians in evaluating alcohol withdrawal. For example, the CIWA-Ar objectifies alcohol withdrawal symptoms in order to guide therapy decisions which allows for an efficient interview while at the same time retaining clinical usefulness, validity, and reliability, ensuring proper care for withdrawal patients, who can be in danger of death.[80]
Causes

A complex combination of genetic and environmental factors influences the risk of the development of alcoholism.[81] Genes that influence the metabolism of alcohol also influence the risk of alcoholism, as can a family history of alcoholism.[82] There is compelling evidence that alcohol use at an early age may influence the expression of genes which increase the risk of alcohol dependence. These genetic and epigenetic results are regarded as consistent with large longitudinal population studies finding that the younger the age of drinking onset, the greater the prevalence of lifetime alcohol dependence.[83][84]
Severe childhood trauma is also associated with a general increase in the risk of drug dependency.[81] Lack of peer and family support is associated with an increased risk of alcoholism developing.[81] Genetics and adolescence are associated with an increased sensitivity to the neurotoxic effects of chronic alcohol misuse. Cortical degeneration due to the neurotoxic effects increases impulsive behaviour, which may contribute to the development, persistence and severity of alcohol use disorders. There is evidence that with abstinence, there is a reversal of at least some of the alcohol induced central nervous system damage.[85] The use of cannabis was associated with later problems with alcohol use.[86] Alcohol use was associated with an increased probability of later use of tobacco and illegal drugs such as cannabis.[87]
Availability
Alcohol is the most available, widely consumed, and widely misused recreational drug. Beer alone is the world's most widely consumed[88] alcoholic beverage; it is the third-most popular drink overall, after water and tea.[89] It is thought by some to be the oldest fermented beverage.[90][91][92][93]
Gender difference
Based on combined data in the US from SAMHSA's 2004–2005 National Surveys on Drug Use & Health, the rate of past-year alcohol dependence or misuse among persons aged 12 or older varied by level of alcohol use: 44.7% of past month heavy drinkers, 18.5% binge drinkers, 3.8% past month non-binge drinkers, and 1.3% of those who did not drink alcohol in the past month met the criteria for alcohol dependence or misuse in the past year. Males had higher rates than females for all measures of drinking in the past month: any alcohol use (57.5% vs. 45%), binge drinking (30.8% vs. 15.1%), and heavy alcohol use (10.5% vs. 3.3%), and males were twice as likely as females to have met the criteria for alcohol dependence or misuse in the past year (10.5% vs. 5.1%).[94] However, because females generally weigh less than males, have more fat and less water in their bodies, and metabolize less alcohol in their esophagus and stomach, they are likely to develop higher blood alcohol levels per drink. Women may also be more vulnerable to liver disease.[95]
Genetic variation
There are genetic variations that affect the risk for alcoholism.[82][81][96][97] Some of these variations are more common in individuals with ancestry from certain areas; for example, Africa, East Asia, the Middle East and Europe. The variants with strongest effect are in genes that encode the main enzymes of alcohol metabolism, ADH1B and ALDH2.[82][96][97] These genetic factors influence the rate at which alcohol and its initial metabolic product, acetaldehyde, are metabolized.[82] They are found at different frequencies in people from different parts of the world.[98][82][99] The alcohol dehydrogenase allele ADH1B*2 causes a more rapid metabolism of alcohol to acetaldehyde, and reduces risk for alcoholism;[82] it is most common in individuals from East Asia and the Middle East. The alcohol dehydrogenase allele ADH1B*3 also causes a more rapid metabolism of alcohol. The allele ADH1B*3 is only found in some individuals of African descent and certain Native American tribes. African Americans and Native Americans with this allele have a reduced risk of developing alcoholism.[82][99][100] Native Americans, however, have a significantly higher rate of alcoholism than average; risk factors such as cultural environmental effects (e.g. trauma) have been proposed to explain the higher rates.[101][102] The aldehyde dehydrogenase allele ALDH2*2 greatly reduces the rate at which acetaldehyde, the initial product of alcohol metabolism, is removed by conversion to acetate; it greatly reduces the risk for alcoholism.[82][98]
A genome-wide association study (GWAS) of more than 100,000 human individuals identified variants of the gene KLB, which encodes the transmembrane protein β-Klotho, as highly associated with alcohol consumption. The protein β-Klotho is an essential element in cell surface receptors for hormones involved in modulation of appetites for simple sugars and alcohol.[103] Several large GWAS have found differences in the genetics of alcohol consumption and alcohol dependence, although the two are to some degree related.[96][97][104]
DNA damage
Alcohol-induced DNA damage, when not properly repaired, may have a key role in the neurotoxicity induced by alcohol.[105] Metabolic conversion of ethanol to acetaldehyde can occur in the brain and the neurotoxic effects of ethanol appear to be associated with acetaldehyde induced DNA damages including DNA adducts and crosslinks.[105] In addition to acetaldehyde, alcohol metabolism produces potentially genotoxic reactive oxygen species, which have been demonstrated to cause oxidative DNA damage.[105]
Diagnosis
Definition

Because there is disagreement on the definition of the word alcoholism, it is not a recognized diagnosis, and the use of the term alcoholism is discouraged due to its heavily stigmatized connotations.[17][18] It is classified as alcohol use disorder[2] in the DSM-5[4] or alcohol dependence in the ICD-11.[106] In 1979, the World Health Organization discouraged the use of alcoholism due to its inexact meaning, preferring alcohol dependence syndrome.[107]
Misuse, problem use, abuse, and heavy use of alcohol refer to improper use of alcohol, which may cause physical, social, or moral harm to the drinker.[108] The Dietary Guidelines for Americans, issued by the United States Department of Agriculture (USDA) in 2005, defines "moderate use" as no more than two alcoholic beverages a day for men and no more than one alcoholic beverage a day for women.[109] The National Institute on Alcohol Abuse and Alcoholism (NIAAA) defines binge drinking as the amount of alcohol leading to a blood alcohol content (BAC) of 0.08, which, for most adults, would be reached by consuming five drinks for men or four for women over a two-hour period. According to the NIAAA, men may be at risk for alcohol-related problems if their alcohol consumption exceeds 14 standard drinks per week or 4 drinks per day, and women may be at risk if they have more than 7 standard drinks per week or 3 drinks per day. It defines a standard drink as one 12-ounce bottle of beer, one 5-ounce glass of wine, or 1.5 ounces of distilled spirits.[110] Despite this risk, a 2014 report in the National Survey on Drug Use and Health found that only 10% of either "heavy drinkers" or "binge drinkers" defined according to the above criteria also met the criteria for alcohol dependence, while only 1.3% of non-binge drinkers met the criteria. An inference drawn from this study is that evidence-based policy strategies and clinical preventive services may effectively reduce binge drinking without requiring addiction treatment in most cases.[111]
Alcoholism
The term alcoholism is commonly used amongst laypeople, but the word is poorly defined. Despite the imprecision inherent in the term, there have been attempts to define how the word alcoholism should be interpreted when encountered. In 1992, it was defined by the National Council on Alcoholism and Drug Dependence (NCADD) and ASAM as "a primary, chronic disease characterized by impaired control over drinking, preoccupation with the drug alcohol, use of alcohol despite adverse consequences, and distortions in thinking."[112] MeSH has had an entry for alcoholism since 1999, and references the 1992 definition.[113]
The WHO calls alcoholism "a term of long-standing use and variable meaning", and use of the term was disfavored by a 1979 WHO expert committee.
In professional and research contexts, the term alcoholism is not currently favored, but rather alcohol abuse, alcohol dependence, or alcohol use disorder are used.[4][2] Talbot (1989) observes that alcoholism in the classical disease model follows a progressive course: if people continue to drink, their condition will worsen. This will lead to harmful consequences in their lives, physically, mentally, emotionally, and socially.[114] Johnson (1980) proposed that the emotional progression of the addicted people's response to alcohol has four phases. The first two are considered "normal" drinking and the last two are viewed as "typical" alcoholic drinking.[114] Johnson's four phases consist of:
- Learning the mood swing. People are introduced to alcohol (in some cultures this can happen at a relatively young age), and they enjoy the happy feeling it produces. At this stage, there is no emotional cost.
- Seeking the mood swing. People will drink to regain that happy feeling in phase 1; the drinking will increase as more alcohol is required to achieve the same effect. Again at this stage, there are no significant consequences.
- At the third stage there are physical and social consequences such as hangovers, family problems, and work problems. People will continue to drink excessively, disregarding the problems.
- The fourth stage can be detrimental with a risk for premature death. People in this phase now drink to feel normal and block out the feelings of overwhelming guilt, remorse, anxiety, and shame they experience when sober.[114]
DSM and ICD
In the United States, the Diagnostic and Statistical Manual of Mental Disorders (DSM) is the most common diagnostic guide for substance use disorders, whereas most countries use the International Classification of Diseases (ICD) for diagnostic (and other) purposes. The two manuals use similar but not identical nomenclature to classify alcohol problems.
| Manual | Nomenclature | Definition |
|---|---|---|
| DSM-IV | Alcohol abuse, or Alcohol dependence |
|
| DSM-5 | Alcohol use disorder | "A problematic pattern of alcohol use leading to clinically significant impairment or distress, as manifested by [two or more symptoms out of a total of 12], occurring within a 12-month period ...."[119] |
| ICD-10 | Alcohol harmful use, or Alcohol dependence syndrome | Definitions are similar to that of the DSM-IV. The World Health Organization uses the term "alcohol dependence syndrome" rather than alcoholism.[107] The concept of "harmful use" (as opposed to "abuse") was introduced in 1992's ICD-10 to minimize underreporting of damage in the absence of dependence.[116] The term "alcoholism" was removed from ICD between ICD-8/ICDA-8 and ICD-9.[120] |
| ICD-11 | Episode of harmful use of alcohol, Harmful pattern of use of alcohol, or Alcohol dependence |
|
Social barriers
Attitudes and social stereotypes can create barriers to the detection and treatment of alcohol use disorder. This is more of a barrier for women than men.[why?] Fear of stigmatization may lead women to deny that they have a medical condition, to hide their drinking, and to drink alone. This pattern, in turn, leads family, physicians, and others to be less likely to suspect that a woman they know has alcohol use disorder.[47] In contrast, reduced fear of stigma may lead men to admit that they are having a medical condition, to display their drinking publicly, and to drink in groups. This pattern, in turn, leads family, physicians, and others to be more likely to suspect that a man they know is someone with an alcohol use disorder.[66]
Screening
Screening is recommended among those over the age of 18.[124] Several tools may be used to detect a loss of control of alcohol use. These tools are mostly self-reports in questionnaire form. Another common theme is a score or tally that sums up the general severity of alcohol use.[125]
The CAGE questionnaire, named for its four questions, is one such example that may be used to screen patients quickly in a doctor's office.
Two "yes" responses indicate that the respondent should be investigated further.
The questionnaire asks the following questions:
- The CAGE questionnaire has demonstrated a high effectiveness in detecting alcohol-related problems; however, it has limitations in people with less severe alcohol-related problems, white women and college students.[128]
Other tests are sometimes used for the detection of alcohol dependence, such as the Alcohol Dependence Data Questionnaire, which is a more sensitive diagnostic test than the CAGE questionnaire. It helps distinguish a diagnosis of alcohol dependence from one of heavy alcohol use.[129] The Michigan Alcohol Screening Test (MAST) is a screening tool for alcoholism widely used by courts to determine the appropriate sentencing for people convicted of alcohol-related offenses,[130] driving under the influence being the most common. The Alcohol Use Disorders Identification Test (AUDIT), a screening questionnaire developed by the World Health Organization, is unique in that it has been validated in six countries and is used internationally. Like the CAGE questionnaire, it uses a simple set of questions – a high score earning a deeper investigation.[131] The Paddington Alcohol Test (PAT) was designed to screen for alcohol-related problems amongst those attending Accident and Emergency departments. It concords well with the AUDIT questionnaire but is administered in a fifth of the time.[132]
Urine and blood tests
There are reliable tests for the actual use of alcohol, one common test being that of blood alcohol content (BAC).[133] These tests do not differentiate people with alcohol use disorders from people without; however, long-term heavy drinking does have a few recognizable effects on the body, including:[citation needed]
- Macrocytosis (enlarged MCV)
- Elevated GGT
- Moderate elevation of AST and ALT and an AST: ALT ratio of 2:1
- High carbohydrate deficient transferrin (CDT)
With regard to alcoholism, BAC is useful to judge alcohol tolerance, which in turn is a sign of alcoholism.[4] Electrolyte and acid-base abnormalities including hypokalemia, hypomagnesemia, hyponatremia, hyperuricemia, metabolic acidosis, and respiratory alkalosis are common in people with alcohol use disorders.[5]
However, none of these blood tests for biological markers is as sensitive as screening questionnaires.
Prevention
The World Health Organization, the European Union and other regional bodies, national governments and parliaments have formed alcohol policies in order to reduce the harm of alcoholism.[134][135]
Increasing the age at which alcohol can be purchased, and banning or restricting alcohol beverage advertising are common methods to reduce alcohol use among adolescents and young adults in particular, see Alcoholism in adolescence. Another common method of alcoholism prevention is taxation of alcohol products – increasing price of alcohol by 10% is linked with reduction of consumption of up to 10%.[136]
Credible, evidence-based educational campaigns in the mass media about the consequences of alcohol misuse have been recommended. Guidelines for parents to prevent alcohol misuse amongst adolescents, and for helping young people with mental health problems have also been suggested.[137]
Because alcohol is often used for self-medication of conditions like anxiety temporarily, prevention of alcoholism may be attempted by reducing the severity or prevalence of stress and anxiety in individuals.[4][7]
Management
Treatments are varied because there are multiple perspectives of alcoholism. Those who approach alcoholism as a medical condition or disease recommend differing treatments from, for instance, those who approach the condition as one of social choice. Most treatments focus on helping people discontinue their alcohol intake, followed up with life training and/or social support to help them resist a return to alcohol use. Since alcoholism involves multiple factors which encourage a person to continue drinking, they must all be addressed to successfully prevent a relapse. An example of this kind of treatment is detoxification followed by a combination of supportive therapy, attendance at self-help groups, and ongoing development of coping mechanisms. Much of the treatment community for alcoholism supports an abstinence-based zero tolerance approach popularized by the 12 step program of Alcoholics Anonymous; however, some prefer a harm-reduction approach.[138]
Cessation of alcohol intake
Medical treatment for alcohol detoxification usually involves administration of a benzodiazepine, in order to ameliorate alcohol withdrawal syndrome's adverse impact.[139][140] The addition of phenobarbital improves outcomes if benzodiazepine administration lacks the usual efficacy, and phenobarbital alone might be an effective treatment.[141] Propofol also might enhance treatment for individuals showing limited therapeutic response to a benzodiazepine.[142][143] Individuals who are only at risk of mild to moderate withdrawal symptoms can be treated as outpatients. Individuals at risk of a severe withdrawal syndrome as well as those who have significant or acute comorbid conditions can be treated as inpatients. Direct treatment can be followed by a treatment program for alcohol dependence or alcohol use disorder to attempt to reduce the risk of relapse.[9] Experiences following alcohol withdrawal, such as depressed mood and anxiety, can take weeks or months to abate while other symptoms persist longer due to persisting neuroadaptations.[77]
Psychological

Various forms of group therapy or psychotherapy are sometimes used to encourage and support abstinence from alcohol, or to reduce alcohol consumption to levels that are not associated with adverse outcomes. Mutual-aid group-counseling is an approach used to facilitate relapse prevention.[8] Alcoholics Anonymous was one of the earliest organizations formed to provide mutual peer support and non-professional counseling, however the effectiveness of Alcoholics Anonymous is disputed.[144] A 2020 Cochrane review concluded that Twelve-Step Facilitation (TSF) probably achieves outcomes such as fewer drinks per drinking day, however evidence for such a conclusion comes from low to moderate certainty evidence "so should be regarded with caution".[145] Others include LifeRing Secular Recovery, SMART Recovery, Women for Sobriety, and Secular Organizations for Sobriety.[146]
Manualized[147] Twelve Step Facilitation (TSF) interventions (i.e. therapy which encourages active, long-term Alcoholics Anonymous participation) for Alcohol Use Disorder lead to higher abstinence rates, compared to other clinical interventions and to wait-list control groups.[148]
Moderate drinking
Moderate drinking amongst people with alcohol dependence—often termed 'controlled drinking'—has been subject to significant controversy.[149] Indeed, much of the skepticism toward the viability of moderate drinking goals stems from historical ideas about 'alcoholism', now replaced with 'alcohol use disorder' or alcohol dependence in most scientific contexts. A 2021 meta-analysis and systematic review of controlled drinking covering 22 studies concluded controlled drinking was a 'non-inferior' outcome to abstinence for many drinkers.[150]
Rationing and moderation programs such as Moderation Management and DrinkWise do not mandate complete abstinence. While most people with alcohol use disorders are unable to limit their drinking in this way, some return to moderate drinking. A 2002 US study by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) showed that 17.7% of individuals diagnosed as alcohol dependent more than one year prior returned to low-risk drinking. This group, however, showed fewer initial symptoms of dependency.[151]
A follow-up study, using the same subjects that were judged to be in remission in 2001–2002, examined the rates of return to problem drinking in 2004–2005. The study found abstinence from alcohol was the most stable form of remission for recovering alcoholics.[152] There was also a 1973 study showing chronic alcoholics drinking moderately again,[153] but a 1982 follow-up showed that 95% of subjects were not able to maintain drinking in moderation over the long term.[154][155] Another study was a long-term (60 year) follow-up of two groups of alcoholic men which concluded that "return to controlled drinking rarely persisted for much more than a decade without relapse or evolution into abstinence."[156] Internet based measures appear to be useful at least in the short term.[157]
Medications
In the United States there are four approved medications for alcoholism: acamprosate, two methods of using naltrexone and disulfiram.[158]
- Acamprosate may stabilise the brain chemistry that is altered due to alcohol dependence via antagonising the actions of glutamate, a neurotransmitter which is hyperactive in the post-withdrawal phase.[159] By reducing excessive NMDA activity which occurs at the onset of alcohol withdrawal, acamprosate can reduce or prevent alcohol withdrawal related neurotoxicity.[160] Acamprosate reduces the risk of relapse amongst alcohol-dependent persons.[161][162]
- Naltrexone is a competitive antagonist for opioid receptors, effectively blocking the effects of endorphins and opioids. Naltrexone is used to decrease cravings for alcohol and encourage abstinence. Alcohol causes the body to release endorphins, which in turn release dopamine and activate the reward pathways; hence in the body Naltrexone reduces the pleasurable effects from consuming alcohol.[163] Evidence supports a reduced risk of relapse among alcohol-dependent persons and a decrease in excessive drinking.[162] Nalmefene also appears effective and works in a similar manner.[162]
- Disulfiram prevents the elimination of acetaldehyde, a chemical the body produces when breaking down ethanol. Acetaldehyde itself is the cause of many hangover symptoms from alcohol use. The overall effect is discomfort when alcohol is ingested: an extremely rapid and long-lasting, uncomfortable hangover.
Several other drugs are also used and many are under investigation.
- Benzodiazepines, while useful in the management of acute alcohol withdrawal, if used long-term can cause a worse outcome in alcoholism. Alcoholics on chronic benzodiazepines have a lower rate of achieving abstinence from alcohol than those not taking benzodiazepines. This class of drugs is commonly prescribed to alcoholics for insomnia or anxiety management.[164] Initiating prescriptions of benzodiazepines or sedative-hypnotics in individuals in recovery has a high rate of relapse with one author reporting more than a quarter of people relapsed after being prescribed sedative-hypnotics. Those who are long-term users of benzodiazepines should not be withdrawn rapidly, as severe anxiety and panic may develop, which are known risk factors for alcohol use disorder relapse. Taper regimes of 6–12 months have been found to be the most successful, with reduced intensity of withdrawal.[165][166]
- Calcium carbimide works in the same way as disulfiram; it has an advantage in that the occasional adverse effects of disulfiram, hepatotoxicity and drowsiness, do not occur with calcium carbimide.[167]
- Ondansetron and topiramate are supported by tentative evidence in people with certain genetic patterns.[168][169] Evidence for ondansetron is stronger in people who have recently started to abuse alcohol.[168] Topiramate is a derivative of the naturally occurring sugar monosaccharide D-fructose. Review articles characterize topiramate as showing "encouraging",[168] "promising",[168] "efficacious",[170] and "insufficient"[171] results in the treatment of alcohol use disorders.
Evidence does not support the use of selective serotonin reuptake inhibitors (SSRIs), tricyclic antidepressants (TCAs), antipsychotics, or gabapentin.[162]
Research
Topiramate, a derivative of the naturally occurring sugar monosaccharide D-fructose, has been found effective in helping alcoholics quit or cut back on the amount they drink. Evidence suggests that topiramate antagonizes excitatory glutamate receptors, inhibits dopamine release, and enhances inhibitory gamma-aminobutyric acid function. A 2008 review of the effectiveness of topiramate concluded that the results of published trials are promising, however as of 2008, data was insufficient to support using topiramate in conjunction with brief weekly compliance counseling as a first-line agent for alcohol dependence.[172] A 2010 review found that topiramate may be superior to existing alcohol pharmacotherapeutic options. Topiramate effectively reduces craving and alcohol withdrawal severity as well as improving quality-of-life-ratings.[173]
Baclofen, a GABAB receptor agonist, is under study for the treatment of alcoholism.[174] According to a 2017 Cochrane Systematic Review, there is insufficient evidence to determine the effectiveness or safety for the use of baclofen for withdrawal symptoms in alcoholism.[175] Psilocybin-assisted psychotherapy is under study for the treatment of patients with alcohol use disorder.[176][177]
Dual addictions and dependencies
Alcoholics may also require treatment for other psychotropic drug addictions and drug dependencies. The most common dual dependence syndrome with alcohol dependence is benzodiazepine dependence, with studies showing 10–20% of alcohol-dependent individuals had problems of dependence and/or misuse problems of benzodiazepine drugs such as diazepam or clonazepam. These drugs are, like alcohol, depressants. Benzodiazepines may be used legally, if they are prescribed by doctors for anxiety problems or other mood disorders, or they may be purchased as illegal drugs. Benzodiazepine use increases cravings for alcohol and the volume of alcohol consumed by problem drinkers.[178] Benzodiazepine dependency requires careful reduction in dosage to avoid benzodiazepine withdrawal syndrome and other health consequences. Dependence on other sedative-hypnotics such as zolpidem and zopiclone as well as opiates and illegal drugs is common in alcoholics. Alcohol itself is a sedative-hypnotic and is cross-tolerant with other sedative-hypnotics such as barbiturates, benzodiazepines and nonbenzodiazepines. Dependence upon and withdrawal from sedative-hypnotics can be medically severe and, as with alcohol withdrawal, there is a risk of psychosis or seizures if not properly managed.[179]
Epidemiology
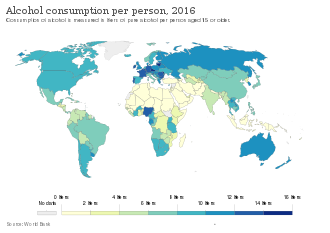
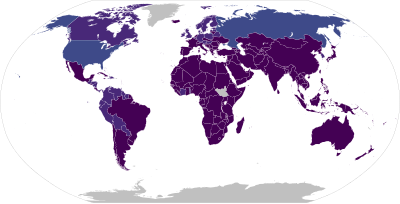
The World Health Organization estimates that as of 2016[update] there are about 380 million people with alcoholism worldwide (5.1% of the population over 15 years of age),[12][13] with it being most common among males and young adults.[4] Geographically, it is least common in Africa (1.1% of the population) and has the highest rates in Eastern Europe (11%).[4]
As of 2015[update] in the United States, about 17 million (7%) of adults and 0.7 million (2.8%) of those age 12 to 17 years of age are affected.[14] About 12% of American adults have had an alcohol dependence problem at some time in their life.[181]
In the United States and Western Europe, 10–20% of men and 5–10% of women at some point in their lives will meet criteria for alcoholism.[182] In England, the number of "dependent drinkers" was calculated as over 600,000 in 2019.[183] Estonia had the highest death rate from alcohol in Europe in 2015 at 8.8 per 100,000 population.[184] In the United States, 30% of people admitted to hospital have a problem related to alcohol.[185]
Within the medical and scientific communities, there is a broad consensus regarding alcoholism as a disease state. For example, the American Medical Association considers alcohol a drug and states that "drug addiction is a chronic, relapsing brain disease characterized by compulsive drug seeking and use despite often devastating consequences. It results from a complex interplay of biological vulnerability, environmental exposure, and developmental factors (e.g., stage of brain maturity)."[186] Alcoholism has a higher prevalence among men, though, in recent decades, the proportion of female alcoholics has increased.[48] Current evidence indicates that in both men and women, alcoholism is 50–60% genetically determined, leaving 40–50% for environmental influences.[187] Most alcoholics develop alcoholism during adolescence or young adulthood.[81]
Prognosis
Alcoholism often reduces a person's life expectancy by around ten years.[21] The most common cause of death in alcoholics is from cardiovascular complications.[188] There is a high rate of suicide in chronic alcoholics, which increases the longer a person drinks. Approximately 3–15% of alcoholics die by suicide,[189] and research has found that over 50% of all suicides are associated with alcohol or drug dependence. This is believed to be due to alcohol causing physiological distortion of brain chemistry, as well as social isolation. Suicide is also common in adolescent alcohol abusers. Research in 2000 found that 25% of suicides in adolescents were related to alcohol abuse.[190]
Among those with alcohol dependence after one year, some met the criteria for low-risk drinking, even though only 26% of the group received any treatment, with the breakdown as follows: 25% were found to be still dependent, 27% were in partial remission (some symptoms persist), 12% asymptomatic drinkers (consumption increases chances of relapse) and 36% were fully recovered – made up of 18% low-risk drinkers plus 18% abstainers.[191] In contrast, however, the results of a long-term (60-year) follow-up of two groups of alcoholic men indicated that "return to controlled drinking rarely persisted for much more than a decade without relapse or evolution into abstinence....return-to-controlled drinking, as reported in short-term studies, is often a mirage."[156]
History

Historically the name dipsomania was coined by German physician C. W. Hufeland in 1819 before it was superseded by alcoholism.[192][193] That term now has a more specific meaning.[194] The term alcoholism was first used by Swedish physician Magnus Huss in an 1852 publication to describe the systemic adverse effects of alcohol.[16]
Alcohol has a long history of use and misuse throughout recorded history. Biblical, Egyptian and Babylonian sources record the history of abuse and dependence on alcohol. In some ancient cultures alcohol was worshiped and in others, its misuse was condemned. Excessive alcohol misuse and drunkenness were recognized as causing social problems even thousands of years ago. However, the defining of habitual drunkenness as it was then known as and its adverse consequences were not well established medically until the 18th century. In 1647 a Greek monk named Agapios was the first to document that chronic alcohol misuse was associated with toxicity to the nervous system and body which resulted in a range of medical disorders such as seizures, paralysis, and internal bleeding. In the 1910s and 1920s, the effects of alcohol misuse and chronic drunkenness boosted membership of the temperance movement and led to the prohibition of alcohol in many countries in North America and the Nordic countries, nationwide bans on the production, importation, transportation, and sale of alcoholic beverages that generally remained in place until the late 1920s or early 1930s; these policies resulted in the decline of death rates from cirrhosis and alcoholism.[195] In 2005, alcohol dependence and misuse was estimated to cost the US economy approximately 220 billion dollars per year, more than cancer and obesity.[196]
Society and culture
The various health problems associated with long-term alcohol consumption are generally perceived as detrimental to society; for example, money due to lost labor-hours, medical costs due to injuries due to drunkenness and organ damage from long-term use, and secondary treatment costs, such as the costs of rehabilitation facilities and detoxification centers. Alcohol use is a major contributing factor for head injuries, motor vehicle injuries (27%), interpersonal violence (18%), suicides (18%), and epilepsy (13%).[197] Beyond the financial costs that alcohol consumption imposes, there are also significant social costs to both the alcoholic and their family and friends.[67] For instance, alcohol consumption by a pregnant woman can lead to an incurable and damaging condition known as fetal alcohol syndrome, which often results in cognitive deficits, mental health problems, an inability to live independently and an increased risk of criminal behaviour, all of which can cause emotional stress for parents and caregivers.[198][199] Estimates of the economic costs of alcohol misuse, collected by the World Health Organization, vary from 1–6% of a country's GDP.[200] One Australian estimate pegged alcohol's social costs at 24% of all drug misuse costs; a similar Canadian study concluded alcohol's share was 41%.[201] One study quantified the cost to the UK of all forms of alcohol misuse in 2001 as £18.5–20 billion.[183][202] All economic costs in the United States in 2006 have been estimated at $223.5 billion.[203]
The idea of hitting rock bottom refers to an experience of stress that can be attributed to alcohol misuse.[204] There is no single definition for this idea, and people may identify their own lowest points in terms of lost jobs, lost relationships, health problems, legal problems, or other consequences of alcohol misuse.[205] The concept is promoted by 12-step recovery groups and researchers using the transtheoretical model of motivation for behavior change.[205] The first use of this slang phrase in the formal medical literature appeared in a 1965 review in the British Medical Journal,[205] which said that some men refused treatment until they "hit rock bottom", but that treatment was generally more successful for "the alcohol addict who has friends and family to support him" than for impoverished and homeless addicts.[206]
Stereotypes of alcoholics are often found in fiction and popular culture. The "town drunk" is a stock character in Western popular culture. Stereotypes of drunkenness may be based on racism or xenophobia, as in the fictional depiction of the Irish as heavy drinkers.[207] Studies by social psychologists Stivers and Greeley attempt to document the perceived prevalence of high alcohol consumption amongst the Irish in America.[208] Alcohol consumption is relatively similar between many European cultures, the United States, and Australia. In Asian countries that have a high gross domestic product, there is heightened drinking compared to other Asian countries, but it is nowhere near as high as it is in other countries like the United States. It is also inversely seen, with countries that have very low gross domestic product showing high alcohol consumption.[209] In a study done on Korean immigrants in Canada, they reported alcohol was typically an integral part of their meal but is the only time solo drinking should occur. They also generally believe alcohol is necessary at any social event, as it helps conversations start.[210]
Peyote, a psychoactive agent, has even shown promise in treating alcoholism. Alcohol had actually replaced peyote as Native Americans' psychoactive agent of choice in rituals when peyote was outlawed.[211]
See also
Notes
References
- ^ "Alcoholism MeSH Descriptor Data 2020". meshb.nlm.nih.gov. Archived from the original on 23 June 2020. Retrieved 9 May 2020.
- ^ a b c d "Alcohol Use Disorder: A Comparison Between DSM–IV and DSM–5". November 2013. Archived from the original on 18 May 2015. Retrieved 9 May 2015.
- ^ a b "Fetal Alcohol Exposure". 14 September 2011. Archived from the original on 4 April 2015. Retrieved 9 May 2015.
- ^ a b c d e f g h i j k l m n o p q r s Diagnostic and statistical manual of mental disorders: DSM-5 (5 ed.). Washington, DC: American Psychiatric Association. 2013. pp. 490–97. ISBN 978-0-89042-554-1.
- ^ a b c d "Alcohol's Effects on the Body". 14 September 2011. Archived from the original on 3 June 2015. Retrieved 9 May 2015.
- ^ Borges G, Bagge CL, Cherpitel CJ, Conner KR, Orozco R, Rossow I (April 2017). "A meta-analysis of acute use of alcohol and the risk of suicide attempt". Psychological Medicine. 47 (5): 949–957. doi:10.1017/S0033291716002841. PMC 5340592. PMID 27928972.
- ^ a b c Moonat S, Pandey SC (2012). "Stress, epigenetics, and alcoholism". Alcohol Research. 34 (4): 495–505. PMC 3860391. PMID 23584115.
- ^ a b c Morgan-Lopez AA, Fals-Stewart W (May 2006). "Analytic complexities associated with group therapy in substance abuse treatment research: problems, recommendations, and future directions". Experimental and Clinical Psychopharmacology. 14 (2): 265–73. doi:10.1037/1064-1297.14.2.265. PMC 4631029. PMID 16756430.
- ^ a b c d e f Blondell RD (February 2005). "Ambulatory detoxification of patients with alcohol dependence". American Family Physician. 71 (3): 495–502. PMID 15712624.
- ^ a b Testino G, Leone S, Borro P (December 2014). "Treatment of alcohol dependence: recent progress and reduction of consumption". Minerva Medica. 105 (6): 447–66. PMID 25392958.
- ^ Kelly JF, Humphreys K, Ferri M (2020). "Alcoholics Anonymous and other 12-step programs for alcohol use disorder". The Cochrane Database of Systematic Reviews. 2020 (3): CD012880. doi:10.1002/14651858.CD012880.pub2. PMC 7065341. PMID 32159228.
- ^ a b c Global status report on alcohol and health 2018 (PDF). World Health Organization. 2018. pp. 72, 80. ISBN 978-92-4-156563-9. Archived (PDF) from the original on 25 July 2019. Retrieved 1 July 2024.
- ^ a b c "World Population Prospects – Population Division". United Nations. Archived from the original on 15 June 2020. Retrieved 1 July 2024.
- ^ a b c d "Alcohol Facts and Statistics". Archived from the original on 18 May 2015. Retrieved 9 May 2015.
- ^ Littrell J (2014). Understanding and Treating Alcoholism Volume I: An Empirically Based Clinician's Handbook for the Treatment of Alcoholism: Volume II: Biological, Psychological, and Social Aspects of Alcohol Consumption and Abuse. Hoboken: Taylor and Francis. p. 55. ISBN 978-1-317-78314-5. Archived from the original on 20 July 2017.
The World Health Organization defines alcoholism as any drinking which results in problems
- ^ a b Alcoholismus chronicus, eller Chronisk alkoholssjukdom. Stockholm und Leipzig. 1852. Retrieved 19 February 2008.
- ^ a b Morris J, Moss AC, Albery IP, Heather N (1 January 2022). "The 'alcoholic other': Harmful drinkers resist problem recognition to manage identity threat". Addictive Behaviors. 124: 107093. doi:10.1016/j.addbeh.2021.107093. PMID 34500234. Archived from the original on 30 March 2024. Retrieved 1 July 2024.
- ^ a b Ashford RD, Brown AM, Curtis B (1 August 2018). "Substance use, recovery, and linguistics: The impact of word choice on explicit and implicit bias". Drug and Alcohol Dependence. 189: 131–138. doi:10.1016/j.drugalcdep.2018.05.005. PMC 6330014. PMID 29913324.
- ^ Rehm J (2011). "The risks associated with alcohol use and alcoholism". Alcohol Research & Health. 34 (2): 135–143. PMC 3307043. PMID 22330211.
- ^ Romeo J, Wärnberg J, Nova E, Díaz LE, Gómez-Martinez S, Marcos A (October 2007). "Moderate alcohol consumption and the immune system: a review". The British Journal of Nutrition. 98 (Suppl 1): S111-5. doi:10.1017/S0007114507838049. PMID 17922947.
- ^ a b c Schuckit MA (November 2014). "Recognition and management of withdrawal delirium (delirium tremens)". The New England Journal of Medicine. 371 (22): 2109–13. doi:10.1056/NEJMra1407298. PMID 25427113. S2CID 205116954. Archived from the original on 13 February 2020. Retrieved 1 July 2024.
- ^ Ritzer G, ed. (15 February 2007). The Blackwell Encyclopedia of Sociology (1 ed.). Wiley. doi:10.1002/9781405165518.wbeosa039.pub2. ISBN 978-1-4051-2433-1. Archived from the original on 1 November 2023. Retrieved 1 July 2024.
- ^ GBD 2013 Mortality Causes of Death Collaborators (January 2015). "Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013". Lancet. 385 (9963): 117–71. doi:10.1016/S0140-6736(14)61682-2. PMC 4340604. PMID 25530442.
- ^ Moonat S, Pandey SC (2012). "[Stress, epigenetics, and alcoholism]". Alcohol Research. 34 (4): 495–505. PMC 3860391. PMID 23584115.
- ^ Agarwal-Kozlowski K, Agarwal DP (April 2000). "[Genetic predisposition for alcoholism]". Therapeutische Umschau. 57 (4): 179–84. doi:10.1024/0040-5930.57.4.179. PMID 10804873.
- ^ Mersy DJ (April 2003). "Recognition of alcohol and substance abuse". American Family Physician. 67 (7): 1529–32. PMID 12722853.
- ^ "Health and Ethics Policies of the AMA House of Delegates" (PDF). June 2008. p. 33. Archived (PDF) from the original on 20 March 2015. Retrieved 10 May 2015.
H-30.997 Dual Disease Classification of Alcoholism: The AMA reaffirms its policy endorsing the dual classification of alcoholism under both the psychiatric and medical sections of the International Classification of Diseases. (Res. 22, I-79; Reaffirmed: CLRPD Rep. B, I-89; Reaffirmed: CLRPD Rep. B, I-90; Reaffirmed by CSA Rep. 14, A-97; Reaffirmed: CSAPH Rep. 3, A-07)
- ^ Higgins-Biddle JC, Babor TF (2018). "A review of the Alcohol Use Disorders Identification Test (AUDIT), AUDIT-C, and USAUDIT for screening in the United States: Past issues and future directions". The American Journal of Drug and Alcohol Abuse. 44 (6): 578–586. doi:10.1080/00952990.2018.1456545. PMC 6217805. PMID 29723083.
- ^ DeVido JJ, Weiss RD (December 2012). "Treatment of the depressed alcoholic patient". Current Psychiatry Reports. 14 (6): 610–8. doi:10.1007/s11920-012-0314-7. PMC 3712746. PMID 22907336.
- ^ Albanese AP (November 2012). "Management of alcohol abuse". Clinics in Liver Disease. 16 (4): 737–62. doi:10.1016/j.cld.2012.08.006. PMID 23101980.
- ^ Kelly JF, Humphreys K, Ferri M (2020). "Alcoholics Anonymous and other 12-step programs for alcohol use disorder". Cochrane Database of Systematic Reviews. 3 (CD012880): 15. doi:10.1002/14651858.CD012880.pub2. PMC 7065341. PMID 32159228.
- ^ Kelly JF, Humphreys K, Ferri M (2020). "Alcoholics Anonymous and other 12-step programs for alcohol use disorder". Cochrane Database of Systematic Reviews. 3 (3): CD012880. doi:10.1002/14651858.CD012880.pub2. PMC 7065341. PMID 32159228.
- ^ Kelly JF, Abry A, Ferri M, Humphreys K (2020). "Alcoholics Anonymous and 12-Step Facilitation Treatments for Alcohol Use Disorder: A Distillation of a 2020 Cochrane Review for Clinicians and Policy Makers". Alcohol and Alcoholism. 55 (6): 641–651. doi:10.1093/alcalc/agaa050. PMC 8060988. PMID 32628263.
- ^ "Alcoholics Anonymous most effective path to alcohol abstinence". 2020. Archived from the original on 20 February 2022. Retrieved 1 July 2024.
- ^ Chambers English Thesaurus. Allied Publishers. p. 175. ISBN 978-81-86062-04-3.
- ^ "Binge Drinking". Center For Disease Control and Prevention. 28 February 2024. Archived from the original on 12 May 2013. Retrieved 28 February 2024.
- ^ a b Hoffman PL, Tabakoff B (July 1996). "Alcohol dependence: a commentary on mechanisms". Alcohol and Alcoholism. 31 (4): 333–40. doi:10.1093/oxfordjournals.alcalc.a008159. PMID 8879279.
- ^ Dunn N, Cook CC (March 1999). "Psychiatric aspects of alcohol misuse". Hospital Medicine. 60 (3): 169–72. doi:10.12968/hosp.1999.60.3.1060. PMID 10476237.
- ^ Wilson R, Kolander CA (2003). Drug abuse prevention: a school and community partnership. Sudbury, MA: Jones and Bartlett. pp. 40–45. ISBN 978-0-7637-1461-1.
- ^ "Biology". The Volume Library. Vol. 1. Nashville, TN: The Southwestern Company. 2009. p. 29. ISBN 978-0-87197-208-8.[permanent dead link]
- ^ a b O'Keefe JH, Bhatti SK, Bajwa A, DiNicolantonio JJ, Lavie CJ (March 2014). "Alcohol and cardiovascular health: the dose makes the poison…or the remedy". Mayo Clinic Proceedings. 89 (3): 382–93. doi:10.1016/j.mayocp.2013.11.005. PMID 24582196.
- ^ American Medical Association (2003). "Duodenal Ulcer". In Leiken JS, Lipsky MS (eds.). Complete Medical Encyclopedia (First ed.). New York: Random House Reference. p. 485. ISBN 978-0-8129-9100-0. Archived from the original on 14 January 2023. Retrieved 1 July 2024.
- ^ Gormley M, Creaney G, Schache A, Ingarfield K, Conway DI (11 November 2022). "Reviewing the epidemiology of head and neck cancer: definitions, trends and risk factors". British Dental Journal. 233 (9): 780–786. doi:10.1038/s41415-022-5166-x. ISSN 0007-0610. PMC 9652141. PMID 36369568.
- ^ Müller D, Koch RD, von Specht H, Völker W, Münch EM (March 1985). "[Neurophysiologic findings in chronic alcohol abuse]". Psychiatrie, Neurologie, und Medizinische Psychologie (in German). 37 (3): 129–32. PMID 2988001.
- ^ Testino G (2008). "Alcoholic diseases in hepato-gastroenterology: a point of view". Hepato-Gastroenterology. 55 (82–83): 371–7. PMID 18613369.
- ^ 10th Special Report to the U.S. Congress on Alcohol and Health Archived 13 September 2012 at the Wayback Machine, 2000, U.S. Department of Health and Human Services, Public Health Service National Institutes of Health, National Institute on Alcohol Abuse and Alcoholism.
- ^ a b c Blum LN, Nielsen NH, Riggs JA (September 1998). "Alcoholism and alcohol abuse among women: report of the Council on Scientific Affairs. American Medical Association". Journal of Women's Health. 7 (7): 861–71. doi:10.1089/jwh.1998.7.861. PMID 9785312.
- ^ a b Walter H, Gutierrez K, Ramskogler K, Hertling I, Dvorak A, Lesch OM (November 2003). "Gender-specific differences in alcoholism: implications for treatment". Archives of Women's Mental Health. 6 (4): 253–8. doi:10.1007/s00737-003-0014-8. PMID 14628177. S2CID 6972064.
- ^ Mihai B, Lăcătuşu C, Graur M (April–June 2008). "[Alcoholic ketoacidosis]". Revista Medico-Chirurgicala a Societatii de Medici Si Naturalisti Din Iasi. 112 (2): 321–6. PMID 19294998.
- ^ Sibaï K, Eggimann P (September 2005). "[Alcoholic ketoacidosis: not rare cause of metabolic acidosis]". Revue Médicale Suisse. 1 (32): 2106, 2108–10, 2112–5. doi:10.53738/REVMED.2005.1.32.2106. PMID 16238232.
- ^ Cederbaum AI (November 2012). "Alcohol metabolism". Clinics in Liver Disease. 16 (4): 667–85. doi:10.1016/j.cld.2012.08.002. PMC 3484320. PMID 23101976.
- ^ a b Bakalkin G (8 July 2008). "Alcoholism-associated molecular adaptations in brain neurocognitive circuits". Eurekalert.org. Archived from the original on 30 November 2011. Retrieved 11 January 2012.
- ^ Oscar-Berman M, Marinkovic K (2003). "Alcoholism and the brain: an overview". Alcohol Research & Health. 27 (2): 125–33. PMC 6668884. PMID 15303622.
- ^ Uekermann J, Daum I (May 2008). "Social cognition in alcoholism: a link to prefrontal cortex dysfunction?". Addiction. 103 (5): 726–35. doi:10.1111/j.1360-0443.2008.02157.x. PMID 18412750.
- ^ Wetterling T, Junghanns K (December 2000). "Psychopathology of alcoholics during withdrawal and early abstinence". European Psychiatry. 15 (8): 483–8. doi:10.1016/S0924-9338(00)00519-8. PMID 11175926. S2CID 24094651.
- ^ Schuckit MA (November 1983). "Alcoholism and other psychiatric disorders". Hospital & Community Psychiatry. 34 (11): 1022–7. doi:10.1176/ps.34.11.1022. PMID 6642446.
- ^ Cowley DS (January 1992). "Alcohol abuse, substance abuse, and panic disorder". The American Journal of Medicine. 92 (1A): 41S – 48S. doi:10.1016/0002-9343(92)90136-Y. PMID 1346485.
- ^ Cosci F, Schruers KR, Abrams K, Griez EJ (June 2007). "Alcohol use disorders and panic disorder: a review of the evidence of a direct relationship". The Journal of Clinical Psychiatry. 68 (6): 874–80. doi:10.4088/JCP.v68n0608. PMID 17592911.
- ^ Grant BF, Harford TC (October 1995). "Comorbidity between DSM-IV alcohol use disorders and major depression: results of a national survey". Drug and Alcohol Dependence. 39 (3): 197–206. doi:10.1016/0376-8716(95)01160-4. PMID 8556968. Archived from the original on 28 November 2020. Retrieved 1 July 2024.
- ^ Kandel DB, Huang FY, Davies M (October 2001). "Comorbidity between patterns of substance use dependence and psychiatric syndromes". Drug and Alcohol Dependence. 64 (2): 233–41. doi:10.1016/S0376-8716(01)00126-0. PMID 11543993.
- ^ Cornelius JR, Bukstein O, Salloum I, Clark D (2003). "Alcohol and psychiatric comorbidity". Recent Developments in Alcoholism. Recent Dev Alcohol. Vol. 16. Kluwer Academic/Plenum Publishers. pp. 361–74. doi:10.1007/0-306-47939-7_24. ISBN 978-0-306-47258-9. ISSN 0738-422X. PMID 12638646.
- ^ Schuckit MA, Tipp JE, Bergman M, Reich W, Hesselbrock VM, Smith TL (July 1997). "Comparison of induced and independent major depressive disorders in 2,945 alcoholics". The American Journal of Psychiatry. 154 (7): 948–57. doi:10.1176/ajp.154.7.948. PMID 9210745.
- ^ Schuckit MA, Tipp JE, Bucholz KK, Nurnberger JI, Hesselbrock VM, Crowe RR, et al. (October 1997). "The life-time rates of three major mood disorders and four major anxiety disorders in alcoholics and controls". Addiction. 92 (10): 1289–304. doi:10.1111/j.1360-0443.1997.tb02848.x. PMID 9489046. S2CID 14958283.
- ^ Schuckit MA, Smith TL, Danko GP, Pierson J, Trim R, Nurnberger JI, et al. (November 2007). "A comparison of factors associated with substance-induced versus independent depressions". Journal of Studies on Alcohol and Drugs. 68 (6): 805–12. doi:10.15288/jsad.2007.68.805. PMID 17960298. S2CID 17528609.
- ^ Schuckit M (June 1983). "Alcoholic patients with secondary depression". The American Journal of Psychiatry. 140 (6): 711–4. doi:10.1176/ajp.140.6.711. PMID 6846629.
- ^ a b c Karrol BR (2002). "Women and alcohol use disorders: a review of important knowledge and its implications for social work practitioners". Journal of Social Work. 2 (3): 337–56. doi:10.1177/146801730200200305. S2CID 73186615.
- ^ a b c McCully C (2004). Goodbye Mr. Wonderful. Alcohol, Addition and Early Recovery. London: Jessica Kingsley Publishers. ISBN 978-1-84310-265-6. Archived from the original on 21 November 2009.
- ^ Isralowitz R (2004). Drug use: a reference handbook. Santa Barbara, CA: ABC-CLIO. pp. 122–23. ISBN 978-1-57607-708-5. Archived from the original on 14 January 2023. Retrieved 1 July 2024.
- ^ Langdana FK (2009). Macroeconomic Policy: Demystifying Monetary and Fiscal Policy (2nd ed.). Springer. p. 81. ISBN 978-0-387-77665-1. Archived from the original on 14 January 2023. Retrieved 1 July 2024.
- ^ Gifford M (2009). Alcoholism (Biographies of Disease). Greenwood Press. pp. 89–91. ISBN 978-0-313-35908-8.
- ^ Schadé JP (2006). The Complete Encyclopedia of Medicine and Health. Foreign Media Books. pp. 132–33. ISBN 978-1-60136-001-4.
- ^ Gold M. "Children of Alcoholics". Psych Central. Archived from the original on 16 November 2011. Retrieved 27 November 2011.
- ^ Galanter M, Kleber HD (2008). The American Psychiatric Publishing Textbook of Substance Abuse Treatment (4th ed.). American Psychiatric Publishing Inc. p. 58. ISBN 978-1-58562-276-4. Archived from the original on 5 February 2023. Retrieved 1 July 2024.
- ^ Dart RC (2003). Medical Toxicology (3rd ed.). Lippincott Williams & Wilkins. pp. 139–40. ISBN 978-0-7817-2845-4.
- ^ Idemudia SO, Bhadra S, Lal H (June 1989). "The pentylenetetrazol-like interoceptive stimulus produced by ethanol withdrawal is potentiated by bicuculline and picrotoxinin". Neuropsychopharmacology. 2 (2): 115–22. doi:10.1016/0893-133X(89)90014-6. PMID 2742726.
- ^ Chastain G (October 2006). "Alcohol, neurotransmitter systems, and behavior". The Journal of General Psychology. 133 (4): 329–35. doi:10.3200/GENP.133.4.329-335. PMID 17128954. S2CID 40043433.
- ^ a b c Heilig M, Egli M, Crabbe JC, Becker HC (April 2010). "Acute withdrawal, protracted abstinence and negative affect in alcoholism: are they linked?". Addiction Biology. 15 (2): 169–84. doi:10.1111/j.1369-1600.2009.00194.x. PMC 3268458. PMID 20148778.
- ^ Johnson BA (2011). Addiction medicine: science and practice. New York: Springer. pp. 301–03. ISBN 978-1-4419-0337-2. Archived from the original on 1 December 2015.
- ^ Breese GR, Sinha R, Heilig M (February 2011). "Chronic alcohol neuroadaptation and stress contribute to susceptibility for alcohol craving and relapse". Pharmacology & Therapeutics. 129 (2): 149–71. doi:10.1016/j.pharmthera.2010.09.007. PMC 3026093. PMID 20951730.
- ^ Sullivan JT, Sykora K, Schneiderman J, Naranjo CA, Sellers EM (November 1989). "Assessment of alcohol withdrawal: the revised clinical institute withdrawal assessment for alcohol scale (CIWA-Ar)" (PDF). British Journal of Addiction. 84 (11): 1353–7. CiteSeerX 10.1.1.489.341. doi:10.1111/j.1360-0443.1989.tb00737.x. PMID 2597811. Archived from the original (PDF) on 10 August 2013. Retrieved 25 October 2017.
- ^ a b c d e Enoch MA (December 2006). "Genetic and environmental influences on the development of alcoholism: resilience vs. risk". Annals of the New York Academy of Sciences. 1094 (1): 193–201. Bibcode:2006NYASA1094..193E. doi:10.1196/annals.1376.019. PMID 17347351. S2CID 248697. Archived from the original on 25 July 2020. Retrieved 1 July 2024.
- ^ a b c d e f g h Edenberg HJ, McClintick JN (December 2018). "Alcohol Dehydrogenases, Aldehyde Dehydrogenases, and Alcohol Use Disorders: A Critical Review". Alcoholism: Clinical and Experimental Research. 42 (12): 2281–2297. doi:10.1111/acer.13904. PMC 6286250. PMID 30320893.
- ^ Agrawal A, Sartor CE, Lynskey MT, Grant JD, Pergadia ML, Grucza R, et al. (December 2009). "Evidence for an interaction between age at first drink and genetic influences on DSM-IV alcohol dependence symptoms". Alcoholism: Clinical and Experimental Research. 33 (12): 2047–56. doi:10.1111/j.1530-0277.2009.01044.x. PMC 2883563. PMID 19764935.
- ^ Crews FT, Vetreno RP, Broadwater MA, Robinson DL (2016). "Adolescent Alcohol Exposure Persistently Impacts Adult Neurobiology and Behavior". Pharmacol Rev. 68 (4): 1074–1109. doi:10.1124/pr.115.012138. PMC 5050442. PMID 27677720.
- ^ Crews FT, Boettiger CA (September 2009). "Impulsivity, frontal lobes and risk for addiction". Pharmacology, Biochemistry, and Behavior. 93 (3): 237–47. doi:10.1016/j.pbb.2009.04.018. PMC 2730661. PMID 19410598.
- ^ Weinberger AH, Platt J, Goodwin RD (April 2016). "Is cannabis use associated with an increased risk of onset and persistence of alcohol use disorders? A three-year prospective study among adults in the United States". Drug and Alcohol Dependence. 161: 363–7. doi:10.1016/j.drugalcdep.2016.01.014. PMC 5028105. PMID 26875671.
- ^ Kirby T, Barry AE (August 2012). "Alcohol as a gateway drug: a study of US 12th graders" (PDF). The Journal of School Health. 82 (8): 371–9. doi:10.1111/j.1746-1561.2012.00712.x. PMID 22712674. Archived (PDF) from the original on 4 June 2016.
- ^ "Volume of World Beer Production". European Beer Guide. Archived from the original on 28 October 2006. Retrieved 17 October 2006.
- ^ Nelson M (2005). The Barbarian's Beverage: A History of Beer in Ancient Europe. Abingdon, Oxon: Routledge. p. 1. ISBN 978-0-415-31121-2. Archived from the original on 14 January 2023. Retrieved 21 September 2010.
- ^ Rudgley R (1993). The Alchemy of Culture: Intoxicants in Society. London: British Museum Press. p. 411. ISBN 978-0-7141-1736-2. Retrieved 13 January 2012.
- ^ Arnold JP (2005). Origin and History of Beer and Brewing: From Prehistoric Times to the Beginning of Brewing Science and Technology. Cleveland, OH: BeerBooks. p. 411. ISBN 978-0-9662084-1-2. Retrieved 13 January 2012.
- ^ Joshua J. Mark (2011). "Beer". Ancient History Encyclopedia. Archived 3 July 2014 at the Wayback Machine.
- ^ McFarland B (2009). World's Best Beers: One Thousand. Sterling Publishing Company, Inc. ISBN 978-1-4027-6694-7.
- ^ "Gender differences in alcohol use and alcohol dependence or abuse: 2004 or 2005." The NSDUH Report. Retrieved 22 June 2012.
- ^ Diagnostic and statistical manual of mental disorders: DSM-5 (5th ed.). Washington: American psychiatric association. 2013. ISBN 978-0-89042-555-8.
- ^ a b c Walters RK, Polimanti R, Johnson EC, McClintick JN, Adams MJ, Adkins AE, et al. (December 2018). "Transancestral GWAS of alcohol dependence reveals common genetic underpinnings with psychiatric disorders". Nature Neuroscience. 21 (12): 1656–1669. doi:10.1038/s41593-018-0275-1. PMC 6430207. PMID 30482948.
- ^ a b c Kranzler HR, Zhou H, Kember RL, Vickers Smith R, Justice AC, Damrauer S, et al. (April 2019). "Genome-wide association study of alcohol consumption and use disorder in 274,424 individuals from multiple populations". Nature Communications. 10 (1): 1499. Bibcode:2019NatCo..10.1499K. doi:10.1038/s41467-019-09480-8. PMC 6445072. PMID 30940813.
- ^ a b Eng MY, Luczak SE, Wall TL (2007). "ALDH2, ADH1B, and ADH1C genotypes in Asians: a literature review". Alcohol Research & Health. 30 (1): 22–7. PMC 3860439. PMID 17718397.
- ^ a b Ehlers CL (2007). "Variations in ADH and ALDH in Southwest California Indians". Alcohol Research & Health. 30 (1): 14–7. PMC 3860438. PMID 17718395.
- ^ Scott DM, Taylor RE (2007). "Health-related effects of genetic variations of alcohol-metabolizing enzymes in African Americans". Alcohol Research & Health. 30 (1): 18–21. PMC 3860436. PMID 17718396.
- ^ Szlemko WJ, Wood JW, Thurman PJ (October 2006). "Native Americans and alcohol: past, present, and future". The Journal of General Psychology. 133 (4): 435–51. doi:10.3200/GENP.133.4.435-451. PMID 17128961. S2CID 43082343.
- ^ Spillane NS, Smith GT (May 2007). "A theory of reservation-dwelling American Indian alcohol use risk". Psychological Bulletin. 133 (3): 395–418. doi:10.1037/0033-2909.133.3.395. PMID 17469984.
- ^ Schumann G, Liu C, O'Reilly P, Gao H, Song P, Xu B, et al. (December 2016). "KLB is associated with alcohol drinking, and its gene product β-Klotho is necessary for FGF21 regulation of alcohol preference". Proceedings of the National Academy of Sciences of the United States of America. 113 (50): 14372–14377. Bibcode:2016PNAS..11314372S. doi:10.1073/pnas.1611243113. PMC 5167198. PMID 27911795. S2CID 4060021.
- ^ Zhou H, Sealock JM, Sanchez-Roige S, Clarke TK, Levey DF, Cheng Z, et al. (2020). "Genome-wide meta-analysis of problematic alcohol use in 435,563 individuals yields insights into biology and relationships with other traits". Nature Neuroscience. 23 (7): 809–818. doi:10.1038/s41593-020-0643-5. ISSN 1097-6256. PMC 7485556. PMID 32451486.
- ^ a b c Kruman II, Henderson GI, Bergeson SE (July 2012). "DNA damage and neurotoxicity of chronic alcohol abuse". Experimental Biology and Medicine. 237 (7): 740–747. doi:10.1258/ebm.2012.011421. PMC 3685494. PMID 22829701.
- ^ "6C40.2 Alcohol dependence". ICD-11 for Mortality and Morbidity Statistics. September 2020. Archived from the original on 1 August 2018. Retrieved 6 December 2020.
- ^ a b "Lexicon of alcohol and drug terms published by the World Health Organization". World Health Organization. Archived from the original on 5 February 2013.
- ^ American Heritage Dictionaries (2006). The American Heritage dictionary of the English language (4 ed.). Boston: Houghton Mifflin. ISBN 978-0-618-70172-8.
To use wrongly or improperly; misuse: abuse alcohol
- ^ "Dietary Guidelines for Americans 2005". health.gov. 2005. Archived from the original on 1 July 2007. Retrieved 28 November 2009. Dietary Guidelines
- ^ "Young Adult Drinking". Alcohol Alert (68). April 2006. Archived from the original on 13 February 2013. Retrieved 18 February 2013.
- ^ Esser MB, Hedden SL, Kanny D, Brewer RD, Gfroerer JC, Naimi TS (November 2014). "Prevalence of alcohol dependence among US adult drinkers, 2009–2011". Preventing Chronic Disease. 11: E206. doi:10.5888/pcd11.140329. PMC 4241371. PMID 25412029.
- ^ Morse RM, Flavin DK (August 1992). "The definition of alcoholism. The Joint Committee of the National Council on Alcoholism and Drug Dependence and the American Society of Addiction Medicine to Study the Definition and Criteria for the Diagnosis of Alcoholism". JAMA. 268 (8): 1012–4. doi:10.1001/jama.1992.03490080086030. PMID 1501306.
- ^ Alcoholism at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
- ^ a b c Thombs DL (1999). Introduction To Addictive Behaviors 2ed. London: The Guildford Press. pp. 64–65.[permanent dead link]
- ^ a b VandenBos GR (2006). APA dictionary of psychology. Washington, DC: American Psychological Association. ISBN 978-1-59147-380-0.
- ^ a b "Diagnostic Criteria for Alcohol Abuse and Dependence – Alcohol Alert No. 30-1995". Archived from the original on 27 March 2010. Retrieved 17 April 2010.
- ^ Martin CS, Chung T, Langenbucher JW (August 2008). "How should we revise diagnostic criteria for substance use disorders in the DSM-V?". Journal of Abnormal Psychology. 117 (3): 561–75. doi:10.1037/0021-843X.117.3.561. PMC 2701140. PMID 18729609.
- ^ "Proposed Revision | APA DSM-5". Archived from the original on 25 March 2010. Retrieved 17 April 2010.
- ^ Diagnostic and statistical manual of mental disorders: DSM-5 (5th ed.). Arlington, VA: American Psychiatric Association. 2013. p. 490. ISBN 978-0-89042-554-1. OCLC 830807378.
- ^ "A System to Convert ICD Diagnostic Codes for Alcohol Research". Archived from the original on 24 April 2009. Retrieved 17 April 2010.
- ^ "6C40.0 Episode of harmful use of alcohol". ICD-11 for Mortality and Morbidity Statistics. World Health Organization. April 2019. Archived from the original on 1 August 2018. Retrieved 16 August 2020.
- ^ "6C40.1 Harmful pattern of use of alcohol". ICD-11 for Mortality and Morbidity Statistics. World Health Organization. April 2019. Archived from the original on 1 August 2018. Retrieved 16 August 2020.
- ^ "6C40.2 Alcohol dependence". ICD-11 for Mortality and Morbidity Statistics. World Health Organization. April 2019. Archived from the original on 1 August 2018. Retrieved 16 August 2020.
- ^ Curry SJ, Krist AH, Owens DK, Barry MJ, Caughey AB, Davidson KW, et al. (November 2018). "Screening and Behavioral Counseling Interventions to Reduce Unhealthy Alcohol Use in Adolescents and Adults: US Preventive Services Task Force Recommendation Statement". JAMA. 320 (18): 1899–1909. doi:10.1001/jama.2018.16789. PMID 30422199.
- ^ Kahan M (April 1996). "Identifying and managing problem drinkers". Canadian Family Physician. 42: 661–71. PMC 2146411. PMID 8653034.
- ^ Ewing JA (October 1984). "Detecting alcoholism. The CAGE questionnaire". JAMA. 252 (14): 1905–7. doi:10.1001/jama.1984.03350140051025. PMID 6471323.
- ^ "CAGE questionnaire – screen for alcohol misuse" (PDF). Archived from the original (PDF) on 28 July 2011.
- ^ Dhalla S, Kopec JA (2007). "The CAGE questionnaire for alcohol misuse: a review of reliability and validity studies". Clinical and Investigative Medicine. 30 (1): 33–41. doi:10.25011/cim.v30i1.447. PMID 17716538.
- ^ Raistrick D, Dunbar G, Davidson R (1983). "Alcohol Dependence Data Questionnaire (SADD)". European Monitoring Centre for Drugs and Drug Addiction. Archived from the original on 21 July 2016.
- ^ "Michigan Alcohol Screening Test". The National Council on Alcoholism and Drug Dependence. Archived from the original on 6 September 2006.
- ^ Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG (2001). "The Alcohol Use Disorders Identification Test; Guidelines for Use in Primary Care" (PDF). World Health Organization. Archived from the original (PDF) on 2 May 2006.
- ^ Smith SG, Touquet R, Wright S, Das Gupta N (September 1996). "Detection of alcohol misusing patients in accident and emergency departments: the Paddington alcohol test (PAT)". Journal of Accident & Emergency Medicine. 13 (5): 308–12. doi:10.1136/emj.13.5.308. PMC 1342761. PMID 8894853.
- ^ Jones AW (2006). "Urine as a biological specimen for forensic analysis of alcohol and variability in the urine-to-blood relationship". Toxicological Reviews. 25 (1): 15–35. doi:10.2165/00139709-200625010-00002. PMID 16856767. S2CID 11117640.
- ^ "Alcohol". World Health Organization. 2010. Archived from the original on 26 February 2010.
- ^ "Alcohol policy in the WHO European Region: current status and the way forward" (PDF). World Health Organization. 12 September 2005. Archived from the original (PDF) on 23 January 2010.
- ^ Elder R, Lawrence B, Ferguson A, Naimi T, Brewer R, Chattopadhyay S, et al. (2010). "The Effectiveness of Tax Policy Interventions for Reducing Excessive Alcohol Consumption and Related Harms". American Journal of Preventive Medicine. 38 (2): 217–229. doi:10.1016/j.amepre.2009.11.005. ISSN 0749-3797. PMC 3735171. PMID 20117579.
- ^ Crews F, He J, Hodge C (February 2007). "Adolescent cortical development: a critical period of vulnerability for addiction". Pharmacology, Biochemistry, and Behavior. 86 (2): 189–99. doi:10.1016/j.pbb.2006.12.001. PMC 11646682. PMID 17222895. S2CID 6925448.
- ^ Gabbard GO (2001). Treatments of psychiatric disorders (3 ed.). Washington, DC: American Psychiatric Press. ISBN 978-0-88048-910-2.
- ^ Holleck JL, Merchant N, Gunderson CG (2019). "Symptom-Triggered Therapy for Alcohol Withdrawal Syndrome: a Systematic Review and Meta-analysis of Randomized Controlled Trials". Journal of General Internal Medicine. 34 (6): 1018–1024. doi:10.1007/s11606-019-04899-7. ISSN 1525-1497. PMC 6544709. PMID 30937668.
- ^ Long D, Long B, Koyfman A (2017). "The emergency medicine management of severe alcohol withdrawal". The American Journal of Emergency Medicine. 35 (7): 1005–1011. doi:10.1016/j.ajem.2017.02.002. ISSN 1532-8171. PMID 28188055. S2CID 42361581.
- ^ Hammond DA, Rowe JM, Wong A, Wiley TL, Lee KC, Kane-Gill SL (2017). "Patient Outcomes Associated With Phenobarbital Use With or Without Benzodiazepines for Alcohol Withdrawal Syndrome: A Systematic Review". Hospital Pharmacy. 52 (9): 607–616. doi:10.1177/0018578717720310. ISSN 0018-5787. PMC 5735736. PMID 29276297.
- ^ Brotherton AL, Hamilton EP, Kloss HG, Hammond DA (2016). "Propofol for Treatment of Refractory Alcohol Withdrawal Syndrome: A Review of the Literature". Pharmacotherapy. 36 (4): 433–442. doi:10.1002/phar.1726. ISSN 1875-9114. PMID 26893017. S2CID 25910118.
- ^ Schmidt KJ, Doshi MR, Holzhausen JM, Natavio A, Cadiz M, Winegardner JE (2016). "Treatment of Severe Alcohol Withdrawal". The Annals of Pharmacotherapy. 50 (5): 389–401. doi:10.1177/1060028016629161. ISSN 1542-6270. PMID 26861990. S2CID 40312054.
- ^ Ferri M, Amato L, Davoli M (19 July 2006). "Alcoholics Anonymous and other twelve-step programmes for alcohol dependence". Cochrane Database of Systematic Reviews (3): CD005032. doi:10.1002/14651858.CD005032.pub2. PMID 16856072.
no experimental studies unequivocally demonstrated the effectiveness of AA or [12-step] approaches for reducing alcohol dependence or problems
- ^ Kelly JF, Humphreys K, Ferri M (11 March 2020). Cochrane Drugs and Alcohol Group (ed.). "Alcoholics Anonymous and other 12-step programs for alcohol use disorder". The Cochrane Database of Systematic Reviews. 2020 (3): CD012880. doi:10.1002/14651858.CD012880.pub2. ISSN 1469-493X. PMC 7065341. PMID 32159228.
- ^ Smith M, Saisan J (2016). "Self-Help Groups for Alcohol Addiction". Archived from the original on 21 May 2015.
- ^ "APA Dictionary of Psychology". dictionary.apa.org. Archived from the original on 27 April 2018. Retrieved 26 January 2022.
manualized therapy – interventions that are performed according to specific guidelines for administration, maximizing the probability of therapy being conducted consistently across settings, therapists, and clients. Also called manual-assisted therapy; manual-based therapy.
- ^ Kelly JF, Humphreys K, Ferri M (March 2020). "Alcoholics Anonymous and other 12-step programs for alcohol use disorder". The Cochrane Database of Systematic Reviews (Systematic review). 3 (3): CD012880. doi:10.1002/14651858.CD012880.pub2. PMC 7065341. PMID 32159228.
- ^ Ashton M, Davies N. "'Dangerous data': drinking after dependence". findings.org.uk. Archived from the original on 6 October 2022. Retrieved 3 March 2023.
- ^ Henssler J, Müller M, Carreira H, Bschor T, Heinz A, Baethge C (August 2021). "Controlled drinking—non-abstinent versus abstinent treatment goals in alcohol use disorder: a systematic review, meta-analysis and meta-regression". Addiction. 116 (8): 1973–1987. doi:10.1111/add.15329. ISSN 0965-2140. PMID 33188563. S2CID 226948754.
- ^ Dawson DA, Grant BF, Stinson FS, Chou PS, Huang B, Ruan WJ (March 2005). "Recovery from DSM-IV alcohol dependence: United States, 2001–2002". Addiction. 100 (3): 281–92. doi:10.1111/j.1360-0443.2004.00964.x. PMID 15733237. S2CID 19679025. Archived from the original on 19 July 2011.
- ^ Dawson DA, Goldstein RB, Grant BF (December 2007). "Rates and correlates of relapse among individuals in remission from DSM-IV alcohol dependence: a 3-year follow-up". Alcoholism: Clinical and Experimental Research. 31 (12): 2036–45. doi:10.1111/j.1530-0277.2007.00536.x. PMID 18034696. Archived from the original on 25 July 2020. Retrieved 1 July 2024.
- ^ Sobell MB, Sobell LC (1973). "Individualized behavior therapy for alcoholics". Behavior Therapy. 4: 49–72. doi:10.1016/S0005-7894(73)80074-7.
- ^ Pendery ML, Maltzman IM, West LJ (July 1982). "Controlled drinking by alcoholics? New findings and a reevaluation of a major affirmative study". Science. 217 (4555): 169–75. Bibcode:1982Sci...217..169P. doi:10.1126/science.7089552. PMID 7089552.
- ^ "Alcoholism Study Under New Attack". The New York Times. 28 June 1982. Archived from the original on 24 June 2020. Retrieved 1 July 2024.
The new article will say that, 10 years later, four of the 20 had died from alcohol-related causes. Eight others were still drinking excessively, six were abstinent but in most cases after multiple hospitalizations, and one was drinking moderately. The alcohol dependence of that last case was also questioned. Another subject, who could not be found, was reported gravely disabled.
- ^ a b Vaillant GE (August 2003). "A 60-year follow-up of alcoholic men". Addiction. 98 (8): 1043–51. doi:10.1046/j.1360-0443.2003.00422.x. PMID 12873238. S2CID 12835128.
- ^ Riper H, Hoogendoorn A, Cuijpers P, Karyotaki E, Boumparis N, Mira A, et al. (December 2018). "Effectiveness and treatment moderators of internet interventions for adult problem drinking: An individual patient data meta-analysis of 19 randomised controlled trials". PLOS Medicine. 15 (12): e1002714. doi:10.1371/journal.pmed.1002714. PMC 6298657. PMID 30562347.
- ^ "Alcohol and Other Drugs". Alcohol Alert (76). National Institute on Alcohol Abuse and Alcoholism. July 2008. Archived from the original on 28 July 2013. Retrieved 11 July 2013.
- ^ Mason BJ, Heyser CJ (January 2010). "The neurobiology, clinical efficacy and safety of acamprosate in the treatment of alcohol dependence". Expert Opinion on Drug Safety. 9 (1): 177–88. doi:10.1517/14740330903512943. PMID 20021295. S2CID 25810236.
- ^ Mason BJ, Heyser CJ (March 2010). "Acamprosate: a prototypic neuromodulator in the treatment of alcohol dependence". CNS & Neurological Disorders Drug Targets. 9 (1): 23–32. doi:10.2174/187152710790966641. PMC 2853976. PMID 20201812.
- ^ Rösner S, Hackl-Herrwerth A, Leucht S, Lehert P, Vecchi S, Soyka M (September 2010). Rösner S (ed.). "Acamprosate for alcohol dependence". The Cochrane Database of Systematic Reviews (Submitted manuscript). 128 (9): CD004332. doi:10.1002/14651858.CD004332.pub2. PMID 20824837. Archived from the original on 8 July 2020. Retrieved 1 July 2024.
- ^ a b c d Jonas DE, Amick HR, Feltner C, Bobashev G, Thomas K, Wines R, et al. (May 2014). "Pharmacotherapy for adults with alcohol use disorders in outpatient settings: a systematic review and meta-analysis". JAMA. 311 (18): 1889–900. doi:10.1001/jama.2014.3628. PMID 24825644.
- ^ Soyka M, Rösner S (November 2008). "Opioid antagonists for pharmacological treatment of alcohol dependence – a critical review". Current Drug Abuse Reviews. 1 (3): 280–91. doi:10.2174/1874473710801030280. PMID 19630726.
- ^ Lindsay SK, Powell GE, eds. (28 July 1998). The Handbook of Clinical Adult Psychology (2nd ed.). Routledge. p. 402. ISBN 978-0-415-07215-1.
- ^ Gitlow S (2006). Substance Use Disorders: A Practical Guide (2nd ed.). Lippincott Williams & Wilkins. pp. 52, 103–21. ISBN 978-0-7817-6998-3. Archived from the original on 14 January 2023. Retrieved 1 July 2024.
- ^ Kushner MG, Abrams K, Borchardt C (March 2000). "The relationship between anxiety disorders and alcohol use disorders: a review of major perspectives and findings". Clinical Psychology Review. 20 (2): 149–71. doi:10.1016/S0272-7358(99)00027-6. PMID 10721495.
- ^ Ogborne AC (June 2000). "Identifying and treating patients with alcohol-related problems". CMAJ. 162 (12): 1705–8. PMC 1232509. PMID 10870503.
- ^ a b c d Soyka M, Müller CA (August 2017). "Pharmacotherapy of alcoholism – an update on approved and off-label medications". Expert Opinion on Pharmacotherapy. 18 (12): 1187–1199. doi:10.1080/14656566.2017.1349098. PMID 28658981. S2CID 23092076.
- ^ Cservenka A, Yardley MM, Ray LA (August 2017). "Review: Pharmacogenetics of alcoholism treatment: Implications of ethnic diversity". The American Journal on Addictions. 26 (5): 516–525. doi:10.1111/ajad.12463. PMC 5484746. PMID 28134463.
- ^ Hammond CJ, Niciu MJ, Drew S, Arias AJ (April 2015). "Anticonvulsants for the treatment of alcohol withdrawal syndrome and alcohol use disorders". CNS Drugs. 29 (4): 293–311. doi:10.1007/s40263-015-0240-4. PMC 5759952. PMID 25895020.
- ^ Pani PP, Trogu E, Pacini M, Maremmani I (February 2014). "Anticonvulsants for alcohol dependence". The Cochrane Database of Systematic Reviews. 2014 (2): CD008544. doi:10.1002/14651858.CD008544.pub2. PMC 10585425. PMID 24523233.
At the current stage of research, evidence supporting the clinical use of anticonvulsants to treat alcohol dependence is insufficient. Results are conditioned by heterogeneity and by the low number and quality of studies comparing anticonvulsants versus other medications. The uncertainty associated with these results leaves to clinicians the need to balance the possible benefits/risks of treatment with anticonvulsants versus other medications as supported by evidence of efficacy.
- ^ Olmsted CL, Kockler DR (October 2008). "Topiramate for alcohol dependence". Ann Pharmacother. 42 (10): 1475–80. doi:10.1345/aph.1L157. ISSN 1060-0280. PMID 18698008. S2CID 27071889.
- ^ Kenna G, Lomastro T, Schiesl A, Leggio L, Swift R (May 2009). "Review of topiramate: an antiepileptic for the treatment of alcohol dependence". Curr Drug Abuse Rev. 2 (2): 135–42. doi:10.2174/1874473710902020135. PMID 19630744.
- ^ Leggio L, Garbutt, JC, Addolorato, G (March 2010). "Effectiveness and safety of baclofen in the treatment of alcohol dependent patients". CNS & Neurological Disorders Drug Targets. 9 (1): 33–44. doi:10.2174/187152710790966614. PMID 20201813.
- ^ Liu J, Wang LN (20 August 2017). "Baclofen for alcohol withdrawal". The Cochrane Database of Systematic Reviews. 8 (8): CD008502. doi:10.1002/14651858.CD008502.pub5. ISSN 1469-493X. PMC 6483686. PMID 28822350.
- ^ Sullivan K (24 August 2022). "Does psilocybin change your brain? How the ingredient in magic mushrooms may ease addiction". NBC News. Archived from the original on 6 September 2022. Retrieved 7 September 2022.
- ^ Bogenschutz (24 August 2022). "Percentage of Heavy Drinking Days Following Psilocybin-Assisted Psychotherapy vs Placebo in the Treatment of Adult Patients With Alcohol Use Disorder – A Randomized Clinical Trial". JAMA Psychiatry. 79 (10): 953–962. doi:10.1001/jamapsychiatry.2022.2096. PMC 9403854. PMID 36001306. S2CID 251766399. Archived from the original on 5 September 2022. Retrieved 7 September 2022.
- ^ Poulos CX, Zack M (November 2004). "Low-dose diazepam primes motivation for alcohol and alcohol-related semantic networks in problem drinkers". Behavioural Pharmacology. 15 (7): 503–12. doi:10.1097/00008877-200411000-00006. PMID 15472572. S2CID 23040302.
- ^ Johansson BA, Berglund M, Hanson M, Pöhlén C, Persson I (November 2003). "Dependence on legal psychotropic drugs among alcoholics". Alcohol and Alcoholism. 38 (6): 613–8. doi:10.1093/alcalc/agg123. PMID 14633651.
- ^ "Alcohol consumption per person". Our World in Data. Archived from the original on 16 March 2020. Retrieved 5 March 2020.
- ^ Hasin DS, Stinson FS, Ogburn E, Grant BF (July 2007). "Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions". Archives of General Psychiatry. 64 (7): 830–42. doi:10.1001/archpsyc.64.7.830. PMID 17606817.
- ^ "alcoholism". Encyclopædia Britannica. 2010. Archived from the original on 2 December 2010.
- ^ a b "Alcohol dependence prevalence in England". GOV.UK. 18 March 2021. Archived from the original on 1 May 2024. Retrieved 1 July 2024.
- ^ Ballas D, Dorling D, Hennig B (2017). The Human Atlas of Europe. Bristol: Policy Press. p. 73. ISBN 978-1-4473-1354-0.[permanent dead link]
- ^ Vonghia L, Leggio L, Ferrulli A, Bertini M, Gasbarrini G, Addolorato G (December 2008). "Acute alcohol intoxication". European Journal of Internal Medicine. 19 (8): 561–7. doi:10.1016/j.ejim.2007.06.033. PMID 19046719.
- ^ Volkow N. "Science of Addiction" (PDF). American Medical Association. Archived (PDF) from the original on 29 June 2011.
- ^ Dick DM, Bierut LJ (April 2006). "The genetics of alcohol dependence". Current Psychiatry Reports. 8 (2): 151–7. doi:10.1007/s11920-006-0015-1. PMID 16539893. S2CID 10535003.
- ^ Zuskin E, Jukić V, Lipozencić J, Matosić A, Mustajbegović J, Turcić N, et al. (December 2006). "[Alcoholism—how it affects health and working capacity]". Arhiv Za Higijenu Rada I Toksikologiju. 57 (4): 413–26. PMID 17265681.
- ^ American Psychiatric Association practice guidelines for the treatment of psychiatric disorders. Arlington, VA: American Psychiatric Association. 2006. p. 1346. ISBN 978-0-89042-385-1. Archived from the original on 29 May 2016.
- ^ O'Connor R, Sheehy N (29 January 2000). Understanding suicidal behaviour. Leicester: BPS Books. pp. 33–37. ISBN 978-1-85433-290-5. Archived from the original on 13 January 2023. Retrieved 1 July 2024.
- ^ The National Institute on Alcohol Abuse and Alcoholism, U.S. Department of Health and Human Services, NIH News (18 January 2005). "2001–2002 Survey Finds That Many Recover From Alcoholism". National Institutes of Health. Archived from the original on 18 August 2006.
- ^ Peters UH (2007). Lexikon Psychiatrie, Psychotherapie, Medizinische Psychologie. Urban Fischer bei Elsev. ISBN 978-3-437-15061-6.
- ^ Valverde M (1998). Diseases of the Will. Cambridge: Cambridge University Press. p. 48. ISBN 978-0-521-64469-3. Archived from the original on 14 January 2023. Retrieved 1 July 2024.
- ^ Tracy SJ (2005). Alcoholism in America: from reconstruction to prohibition. Baltimore: Johns Hopkins University Press. pp. 31–52. ISBN 978-0-8018-8119-0.
- ^ Blocker JS (February 2006). "Did prohibition really work? Alcohol prohibition as a public health innovation". American Journal of Public Health. 96 (2): 233–43. doi:10.2105/AJPH.2005.065409. PMC 1470475. PMID 16380559.
Nevertheless, once Prohibition became the law of the land, many citizens decided to obey it. Referendum results in the immediate post-Volstead period showed widespread support, and the Supreme Court quickly fended off challenges to the new law. Death rates from cirrhosis and alcoholism, alcoholic psychosis hospital admissions, and drunkenness arrests all declined steeply during the latter years of the 1910s, when both the cultural and the legal climate were increasingly inhospitable to drink, and in the early years after National Prohibition went into effect.
- ^ Potter JV (2008). Substances of Abuse. Vol. 2. AFS Publishing Co. pp. 1–13. ISBN 978-1-930327-46-7.
- ^ "Alcohol and health" (PDF). World Health Organization. Archived (PDF) from the original on 25 July 2020. Retrieved 3 May 2020.
- ^ Streissguth AP (2018). Fetal alcohol syndrome: a guide for families and communities. Baltimore: Paul H Brookes Pub. ISBN 978-1-55766-283-5. Archived from the original on 14 January 2023. Retrieved 1 July 2024.
- ^ Gerberding JL, Cordero J, Floyd RL (May 2005). "Fetal Alcohol Syndrome: Guidelines for Referral and Diagnosis" (PDF). US Centers for Disease Control and Prevention. Archived (PDF) from the original on 11 June 2014.
- ^ "Global Status Report on Alcohol 2004" (PDF). World Health Organization. Archived (PDF) from the original on 30 December 2006. Retrieved 3 January 2007.
- ^ "Economic cost of alcohol consumption". World Health Organization Global Alcohol Database. Archived from the original on 18 January 2008. Retrieved 3 January 2007.
- ^ "Q&A: The costs of alcohol". BBC. 19 September 2003. Archived from the original on 19 October 2006.
- ^ Bouchery EE, Harwood HJ, Sacks JJ, Simon CJ, Brewer RD (November 2011). "Economic costs of excessive alcohol consumption in the U.S., 2006" (PDF). American Journal of Preventive Medicine. 41 (5): 516–24. CiteSeerX 10.1.1.460.5582. doi:10.1016/j.amepre.2011.06.045. PMID 22011424. Archived from the original (PDF) on 21 July 2018. Retrieved 12 December 2017.
- ^ "hit rock bottom". TheFreeDictionary.com. Archived from the original on 16 July 2022. Retrieved 16 July 2022.
- ^ a b c Kirouac M, Witkiewitz K (October 2017). "Identifying 'Hitting Bottom' Among Individuals with Alcohol Problems: Development and Evaluation of the Noteworthy Aspects of Drinking Important to Recovery (NADIR)". Substance Use & Misuse. 52 (12): 1602–1615. doi:10.1080/10826084.2017.1293104. PMC 6107067. PMID 28557550.
- ^ "Treatment of Alcohol Addiction". British Medical Journal. 2 (5455): 184–5. July 1965. doi:10.1136/bmj.2.5455.184. PMC 1846501. PMID 20790596.
- ^ "World/Global Alcohol/Drink Consumption". Finfacts Ireland. 2009. Archived from the original on 12 May 2015.
- ^ Stivers R (2000). Hair of the dog: Irish drinking and its American stereotype. New York: Continuum. ISBN 978-0-8264-1218-8.
- ^ Chen CC, Yin SJ (October 2008). "Alcohol abuse and related factors in Asia". International Review of Psychiatry. 20 (5): 425–33. doi:10.1080/09540260802344075. PMID 19012127. S2CID 24571763.
- ^ Kim W (December 2009). "Drinking culture of elderly Korean immigrants in Canada: a focus group study". Journal of Cross-Cultural Gerontology. 24 (4): 339–53. doi:10.1007/s10823-009-9104-z. PMID 19823926. S2CID 28478567.
- ^ French L (2008). "Psychoactive agents and Native American spirituality: Past and present". Contemporary Justice Review. 11 (2): 155–63. doi:10.1080/10282580802058270. S2CID 143549807.